Hearing Evaluation
Diagnostic Audiologic testing
These tests are part of a diagnostic test battery performed by Dr. Veronica Heide to determine the degree and type of your hearing ability. The outcome of these tests determines whether you need medical referral or audiologic habilitation, hearing instruments, use of assistive devices, speech reading lessons, cochlear implant referral, or other therapies.
Outer Ear - (Otoscopy or Video Otoscopy)
Middle Ear - Tympanometry and acoustic reflex measurements
Otoacoustic emission testing (Outer Hair Cell function testing)
Pure-tone air and bone conduction testing (Audiogram) Speech Threshold (the softest level where you can just barely understand speech)
Word recognition testing (evaluates how well you understand words in quiet at a comfortable volume)
Speech-In-Noise Testing (evaluates how well you understand sentences in noise)
As well as other appropriate tests of perception necessary to understand how your ears and hearing system are working.
How hearing works
Outer Ear
Using video otoscopy, you and the audiologist can see if your outer ear canal is partially or fully occluded with earwax. If there is no debris blocking the ear canals, you will be able to clearly see the landmarks of the eardrum (tympanic membrane) and the middle ear bones.
Video Otoscopy
Video Otoscopy of the eardrum
Middle Ear
Middle Ear
The middle ear system is an impedance matching device that helps transform the airborne sound waves efficiently from the outer ear through the middle ear to the inner ear. If there is a problem with the conduction of sound through the middle ear, sound energy will be lost and hearing loss may occur. Middle ear problems are most often medically managed and may include a hole in the eardrum, ear diseases such as middle ear fluid and infections, stiffening of the middle ear bones (otosclerosis) and other mechanical problems. If middle ear problems are detected during the evaluation you will most likely be referred to an otolaryngologist for medical evaluation and to be cleared medically before pursuing hearing devices.
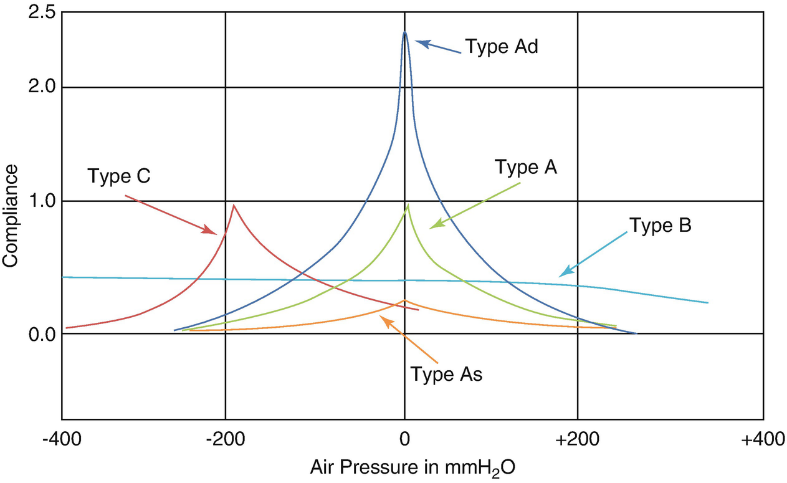
Audiologists can measure how well the middle ear is working using Tympanometry and Acoustic Reflex measurements. Equipment has evolved from measuring the middle ear dynamics from a single frequency to measuring multiple frequency responses from one measurement of reflected sound in the ear canal.
Responses using a single tone measurement
Inner Ear (Hearing and Balance)
Inner Ear
The inner ear is the sensory organ for both hearing and balance. A hearing loss in the inner ear is most often called, “sensorineural loss,” but recently new testing has become available to allow audiologists to differentiate sensory loss from neural loss.
Otoacoustic Emission Testing
Otoacoustic emission testing is often used to evaluate the integrity of the outer hair cells in the inner ear. These microscopic structures are the pre-amplifier of the inner ear elongate and contract to optimize the frequency and intensity of the input signal. Newborn hearing screening has been made possible by the development of equipment to measure outer hair cell function.
Normal outer hair cell structure
Abnormal outer hair cell structures
Measurement of outer hair cell function in infant hearing screening
The top graph shows a robust normal Transient Otoacoustic Emission (TOAE) from an infant, while the bottom graph shows a lack of response from a different infant. Infants are screened in the newborn nursery and referred to a pediatric audiologist for further diagnostic testing if the baby does not pass the screening. Audiologists may also use special computerized tests of the auditory nerve called Auditory Brainstem Response tests to determine if the loss of hearing is due to loss of sensory function or loss of transmission of the auditory signal from the cochlear through the auditory nerve and pathway to the brain.
For more information photographs and videos about ear anatomy go to: http://www.cochlea.eu/en/auditory-brain/brain-stem
Hearing threshold assessment
Harvey Fletcher was a pioneer in audio measurement and sound transmission. His plot below, the Fletcher-Munson curves (later termed equal loudness contours) was derived from his research at Bell Labs to improved telephone audio fidelity. Through this work he pioneered the invention of the first hearing aid and invented stereo sound and demonstrated this at the Chicago World’s Fair much to the delight of those who attended.
Fletcher, H. and Munson, W.A. "Loudness, its definition, measurement and calculation",
Journal of the Acoustical Society of America 5, 82–108 (1933).
The range of frequencies heard by the human ear is between 20 Hz to 20,000 Hz, but the ear is most sensitive in the frequency range from 2000 Hz through 5000 Hz due to resonance of the ear canals and the mechanical advantage provided by the ossicles.
Rather than plot hearing test results on a Fletcher-Munson curve, audiologists took the sound pressure level curve that defined average normal hearing across frequency and termed that average normal hearing with a reference of 0 dB hearing level (HL). So, instead of a curved line, the results are plotted on a straight line referenced to 0 dB HL.
Audiologists typically test the “speech frequencies” between 250 Hz through 8000 Hz in routine diagnostic testing but can extend the range of frequencies tested by using ultra-high frequency headphones calibrated with special audiometric equipment to test as low as 125 Hz and as high as 16,000 Hz.
Conventional Audiogram
Ultra-high frequency audiogram
Degree of Hearing Loss:
-10 to +15 dB – Normal hearing range
15 to 25 dB – Slight loss – misses some soft and distant sounds
30 to 40 dB loss – Mild loss – not aware of soft and distant sounds
45-55 dB loss – Moderate loss – misses many critical speech sounds – often blames others for not speaking clearly.
60-70 dB loss – Moderately severe loss. Misses much of speech without amplification. Generally pleased with hearing instruments.
75 to 90 dB loss – Severe loss - Loss of OHCs and some IHCs results in lack of tuning ability and poor speech understanding even with the best hearing instruments. Speech Reading and the use of ALDs are keys to successful communication.
95 to >110 - Profound loss – Need visual with auditory to communicate effectively. Will benefit from use of captioning, written text, and visual cues. May be a cochlear implant candidate.
Perception
So, while audiologists have automatic tests of the functional integrity of the various components of the hearing mechanism, they still ask patients to respond to tones and speech to measure the perceptions of the individual. The ability to detect sounds across a variety of frequencies and intensities is plotted on an audiogram along with tests that measure speech detection and word comprehension in quiet and in noise.
Speech Understanding
In addition to testing audibility for tones, audiologists will evaluate the softest level at which you can hear speech and also how clearly you understand speech in quiet and speech in noise. The ability to hear well in noise is based on many factors including cognition, neural processing and life experiences. The ability to understand speech in noise can be improved with training.
To learn more about the role of neural processing, cognition, and life experience, visit the website of Nina Kraus, Ph.D.: https://brainvolts.northwestern.edu/
Loudness Discomfort Testing
Loudness discomfort testing will ensure that loud sounds sound loud but not uncomfortably so. This measurement defines the top end of your comfortable listening range and is important not only in hearing instrument programming, but in understanding sound tolerance problems.
Treatment Recommendations
At the conclusion of your diagnostic evaluation, your audiologist will know a lot about your ears and how you perceive sound. By putting the pieces of the diagnostic testing together the audiologist will understand the type of hearing loss and the degree of hearing loss and the impact of these factors on your lifestyle and communication. Based on the diagnostic testing, treatment recommendations are made. These recommendations may include:
Hearing instruments
Continued audiologic follow-up and programming
Assistive listening devices
Aural habilitation such as LACE listening program, music training or personal therapy